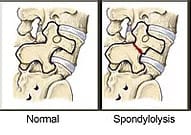
Spondylolysis is a spinal defect or fracture in the bone structure known as the pars interarticularis, which connects the spine's facet joints. This condition is also called "pars defect" or "pars fracture." On the other hand, spondylolisthesis refers to the forward slipping of a vertebral bone, with "listhesis" meaning to slip forward.
Spondylosis Q & A
What is spondylolysis?
How are spondylolysis and spondylolisthesis different from each other?
What symptoms develop if I have spondylolysis?
How do spine specialists diagnose spondylolysis?
How do spine specialists treat spondylolysis?
What is spondylolysis?
Spondylolysis, also called a pars defect or pars fracture, is a stress fracture occurring in the lower back. You’re more likely to develop spondylolysis when you perform repetitive movements that make you bend backward. This bending stresses a specific part of the vertebrae called the pars interarticularis. Pars fractures typically begin in children and adolescents who participate in sports such as football, weightlifting, karate, and gymnastics. A pars fracture that starts in adolescence may not cause symptoms until adulthood.
How are spondylolysis and spondylolisthesis different from each other?
Spondylosis and spondylolisthesis are distinct conditions that affect the spine. Spondylosis refers to degenerative changes in the spine, such as the development of bone spurs and the breakdown of intervertebral discs. On the other hand, spondylolisthesis involves the forward displacement of a vertebra in the spine, often due to a stress fracture in the pars interarticularis, a small bone bridge connecting the facet joints at the back of the spine.
What symptoms develop if I have spondylolysis?
You may not have any symptoms at first, but they can develop over the years as the stress fracture worsens. Then you may experience:
- Lower back pain that feels like a muscle strain
- Pain that’s worse when you’re active
- Increased inward curvature in your lower back
- Pain or tingling that radiates down your legs
- Tight hamstring muscles
- Muscle spasms
In severe cases, spondylolysis weakens the bone so much that the vertebra can slip out of place. This condition, called spondylolisthesis, occurs in about 15% of patients who have untreated spondylolysis.
How do spine specialists diagnose spondylolysis?
Your provider at the Center for the Functional Restoration of the Spine orders diagnostic testing after reviewing your medical history and symptoms and performing a physical examination. Depending on your exam results, you may need an X-ray, CT scan, or MRI to verify spondylolysis and rule out other causes of your symptoms.
How do spine specialists treat spondylolysis?
Your treatment begins with non-surgical therapies such as medication, rest, and physical therapy. You may also need bracing to immobilize your back and give the fracture time to heal. When over-the-counter medications don’t help your pain, your provider may recommend a spinal epidural injection. This injection contains steroids that alleviate your pain by reducing inflammation. If your symptoms still don’t improve after several months of conservative treatment, you may need to consider surgery. Spondylolysis often improves with spinal decompression that takes the pressure off the nerves. This decompression is then followed by a fusion to restore spinal stability. You follow the same treatment plan should your vertebra slip and cause spondylolisthesis. However, you’re more likely to need surgery once a pars fracture progresses to this point. The experienced team at the Center for the Functional Restoration of the Spine offers exceptional treatment for spondylolysis. To schedule an appointment, call or use the online booking feature today.